

An Overview of Greco-Arab and Islamic Herbal Medicine
by Bashar SaadPublished on: 24th June 2020
*** Produced from Chapter 1 of the Book “Greco-Arab and Islamic Herbal Medicine: Traditional System, Ethics, Safety, Efficacy, and Regulatory Issues” By Bashar Saad and Omar Said, Copyright _ 2011 John Wiley & Sons, Inc. *** Introduction Natural products, such as plant, fungal, and bee products, as well as minerals, shells, and certain animal products,...

***
Produced from Chapter 1 of the Book “Greco-Arab and Islamic Herbal Medicine: Traditional System, Ethics, Safety, Efficacy, and Regulatory Issues” By Bashar Saad and Omar Said, Copyright _ 2011 John Wiley & Sons, Inc.
***
Introduction
Natural products, such as plant, fungal, and bee products, as well as minerals, shells, and certain animal products, represent the oldest form of medical treatment. Currently, many of the commonly used drugs are of herbal origin and about 25% of the prescription drugs contain at least one herbal-derived active ingredient or synthetic compound, which mimics a plant-derived compound. There are over 80,000 plants that have medicinal uses throughout the world and usually a specific part of the plant is used for medical preparations such as tablets, infusions, extracts, tinctures, ointments, or creams. The pharmacological action of these medicines is often described in very general terms, such as carminative (an agent that prevents formation of gas in the gastrointestinal tract or facilitates the expulsion of said gas), laxative (an agent that induces bowel movements or loosens the stools), demulcent (an agent that forms a soothing film over a mucous membrane, relieving minor pain and inflammation of the membrane), antitussive (cough suppressants), or antiseptic (antimicrobial substances that are applied to living tissue/skin to reduce the possibility of infection). Unlike synthetic drugs, which usually consist of a single and often synthetic chemical, herbal-based medicines contain multiple constituents.
In the history of science, Arabic medicine, Islamic medicine, Arab–Islamic medicine, Greco-Arab medicine, or Greco-Arab and Islamic medicine are terms that refer to medicine developed during the Golden Age of Muslim civilisation (Figure 1). This civilisation became the centre of brilliant medical developments and innovations, as well as great achievements in astronomy, mathematics, chemistry, philosophy, and artistic culture. Arab and Muslim scholars translated and integrated scientific knowledge of other civilisations into their own innovations. These included the discovery of the immune system, the introduction of microbiological science, and the separation of pharmacological science from medicine. Medicine in general is considered to be one of the most illustrious and best-known achievements that influenced Western medical circles to such an extent that it was included in the curriculum of medical schools up to sixteenth century.
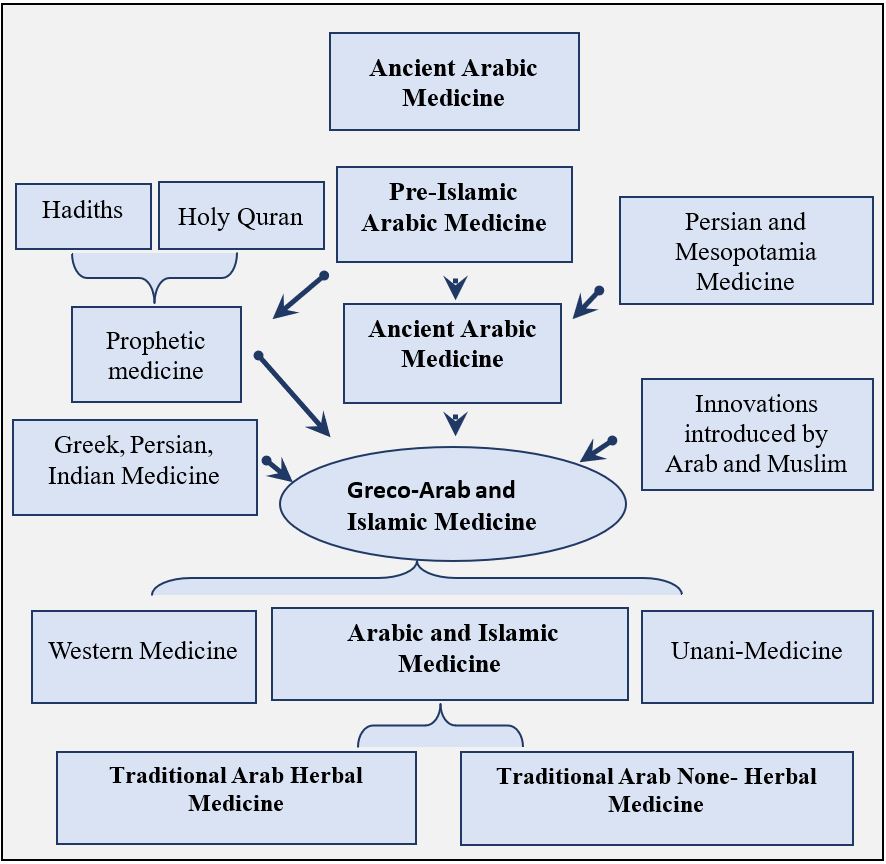
Figure 1. Development of Arab-Islamic medical science. The Babylonians and ancient Egyptians initiated the foundations of medicine with using trial and error. Through trial and error, they laid down the foundations of medicine upon which this field progressed. Both the Mesopotamian and Egyptian lands witnessed fruitful exchange of medicine with Europe over hundreds of years. First, Mesopotamian medicine was transmitted in part to the Greeks, and together with Egyptian medicine, it paved the way for the great Hippocratic reform of the fifth century B.C. Then, during the rise of the Arab-Islamic Empire, Greek medicine was translated to Arabic. The Arabs preserved Greek medicine when most of the original works were lost from Europe. The Arabs improved on Greek medicine as well as made new discoveries over several centuries. In the 13th and 14th centuries Greco-Arab medicine was disseminated to Europe again from Arab capitals such as Cordoba in Andalusia and Baghdad in Iraq. History documents the evolution of medicine, how medical therapies come and go, and how useful procedures become not so useful.
Despite great progress in allopathic medicine, Arab–Islamic medicine has continued to be practiced within the Mediterranean as well as most Muslim countries (Figure 2), where cultural beliefs and religion often lead to self-care or home remedies in rural areas and consultation with traditional healers. In addition, Arab–Islamic therapies are most often utilized by people who have faith in spiritual healers and herbalists. These people are the first to be consulted for problems such as infertility, impotence, diabetes, obesity, epilepsy, psychosomatic troubles, and many other diseases. The popularity of herbal preparations based on Greco-Arab and Islamic medicines has increased worldwide in the past four decades, probably because of the sustainability of this medicine over the years. Other factors include the notion that herbal-based drugs are safe, that they are relatively inexpensive, the restricted access to physicians imposed by managed care, and the adverse effects of synthetic drugs.
Greco-Arab and Islamic medicine was practiced in the Muslim world (Figure 2) including countries other than those in the Middle East, such as Iran, India, Turkey, Maghreb region, and Pakistan [1–10]. India is the only country where Greco-Arab medicine has an official status, usually referred to Unani-Tibb. “Tibb” is an Arabic word meaning “medicine,” while “Unani” is thought to be derived from “Ionan” (meaning Greek), acknowledging the influence of early Greek medicine Islamic medicine. An Unani physician is known as a hakim.
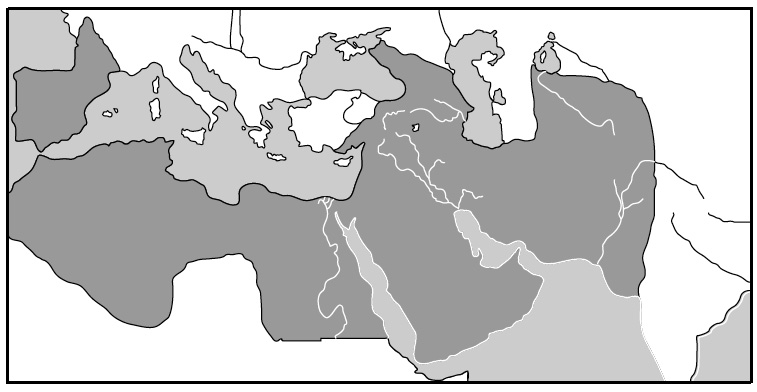
Figure 2. The medieval Muslim world at its largest extension.
However, the Unani medicine currently practiced in the Indo-Pakistan subcontinent is vastly different from its Greco-Arab roots. It benefited from the native medical system or folk medicine in practice at the time in various parts of central and southern Asia, mainly Ayurvedic medicine and Chinese medicine.
The Golden Age of Muslim Civilisation
The development of Muslim civilisation started in the Arabian Peninsula, the homeland of the Arabs. The Peninsula is predominantly deserted and the tribes who inhabited this area were nomadic, that is, they travelled from one grazing land to another. The great unifying power of these nomadic Arabs was clearly the Prophet Muhammad (peace be upon him, PBUH) (570–632) from the Quraysh tribe that ruled Mecca. Though Mecca was a prosperous caravan city, it was still tied to traditional social customs and was governed by the tribal societies of the desert. Each tribe worshipped its own gods in the form of objects from nature but all Arabs worshipped one object in common, the Kaaba, a large black stone at Mecca, which made Mecca significant as a place of worship and pilgrimage. The Prophet was able to unite the nomadic tribes and to create a strong nation, able to defeat the two powerful empires at that time, the Persian and Byzantine Empires.
The Byzantines and Persians were the first to feel the power of unified Arabs. At Yarmuk in 636, the Muslims defeated the Byzantine army (Table 1). Syria fell in 640. A decade later, the Muslims had conquered the entire Persian Empire. Egypt, the Maghreb (North Africa), and Spain were all conquered and under Muslim rule by the 720s. Muslim expansion in Europe ended after their loss of the Battle of Tours in 732. The Muslims not only conquered new lands, but also became scientific innovators through originality and productivity. They preserved the cultures and knowledge of the conquered lands, tolerated religious minorities within land they had conquered, and were careful to protect the purity of their religion, language, and law from any foreign influence.
The first problem after the death of the Prophet was who should be caliph, the spiritual and secular successor to the Prophet (PBUH). The first four caliphs were elected by a tribal council of elders and are referred to as the Rashidun (Guided) Caliphs, ruling from 632 to 661. However, as the state grew, this form of government became increasingly inadequate. In addition, tribal and clan rivalries continued. Finally, the Umayyad clan took over and established the Umayyad Dynasty (661–750). From then on, the dynastic principle of one family choosing the caliph dominated. From the start, the Umayyads were influenced by Byzantine and Persian ruling techniques. Therefore, they instituted some major changes. They moved the capital from Medina in Arabia to a much more central location, Damascus in Syria, created the first Muslim coinage, and also adapted and further developed Byzantine and Persian bureaucratic methods as well as postal communication and transmission of news. In 750, a revolt led by Abbas, a governor of Persia, overthrew the Umayyads and established the Abbasid Dynasty (750–1258). The victorious Abbasids moved their capital to Baghdad to signify a break with the Umayyads. However, the reconstituted Umayyads set up a rival state and put their capital at Cordoba, in Al-Andalus. Even as the Abbasids, in particular the Caliphs Harun al-Rashid (ruled from 786 to 809) and Al-Mamun (ruled from 813 to 833) and their heirs, turned Baghdad into the smartest, most creative, and most modern city of the world, the Umayyads led by Abd Al Rahman I and his heirs set out to do the same thing in Cordoba, Granada, and the other Andalusian cities.
——————————————————————————————————-
TABLE 1 Timeline of Arab Islamic Civilisation
Year Historical Event
570 The Prophet Muhammad is born in Mecca
622 The Prophet and followers emigrate to Medina. The first year of Islamic calendar
632 Death of the Prophet
632 Muslim armies consolidate their power over Arabia
634–644 Muslim forces advance through the Persian and Byzantine empires
636 Battle of Yarmuk. Byzantine emperor Heraclius is defeated by Muslim army in Syria
642 Muslims conquer Byzantine Egypt and expand into North Africa
656 Mohammad’s son-in-law, Ali, succeeds to the leadership of Islam
661–750 Umayyads rule in Damascus
711 Tariq bin Ziyad with a mixed force of Arabs and Berbers invades Spain
712 Muslims advance into Sind (modern-day Pakistan) and Central Asia
725 Muslims occupy Nimes in Southern France
750–945 Abbasids rule in Baghdad
756–929 Umayyad Emirs rule in Spain
762 Al-Mansur founds the city of Baghdad
786 Haroun al-Rashid becomes caliph in Baghdad
792 The first papermaking factory in the Muslim world is built in Baghdad
813–823 Al-Mamun reigns in Baghdad. He founds the House of Wisdom
823 Beginning of Muslim conquest of Sicily
909–1171 Fatimids expand in North Africa
929–1031 Umayyad caliphate reigns in Spain
969 Fatimid conquer Egypt and transfer their capital to Cairo in 973
976 Al-Azhar university is founded in Cairo
1058 Seljuks take Baghdad
1090 Cordoba is taken by Almoravids
1096 First Crusade. Christians rule in Jerusalem in 1099
1145–1232 Almohads rule in Spain
1171 Saladin overthrows the Fatimids in Egypt
1171–1250 Ayyubid Dynasty rules in Egypt and Syria
1187 Saladin returns Jerusalem to Islamic rule
1206–1406 Mongol Empire
1492 Christian Reconquest of Spain
1453–1922 Ottoman Empire
1494–1566 Suleiman I guides the Ottoman Empire to its fullest extent, ranging from Morocco to the Caspian Sea and the Persian Gulf and into Europe through the Balkans to Hungary
1922 End of the Ottoman Empire
All dates given in the table are those of the Christian calendar. Bold entries denote dynastic rule.
—————————————————————————————————————-
Under the Abbasid Caliphs, Islamic civilisation entered a Golden Age. And while in Europe, learning seemed to be at its lowest point, the Arabs created a highly sophisticated civilisation. The period from the seventh to roughly the end of the fifteenth century is known as the Golden Age of Islamic civilisation. During this period, the vigorous desert tribesman from Arabia assimilated and interpreted the Byzantine, Persian, and Indian cultural traditions into their own. Perhaps the most important catalyst was Islam itself that encouraged study, thinking, and discussion, as well as a scientific understanding of the world. Historians of Arab science point to various statements in the Qur’an and in the body of other statements attributed to the Prophet (PBUH): “Even if you must go to China, seek knowledge.” or “Acquire knowledge, because he who acquires it in the way of the Lord performs an act of piety; who speaks of it, praises the Lord; who seeks it, adores God.” Another recognized trigger for the rise of Arab intellect was the acknowledged intellectual traditions of the older societies that fell under Arab and Muslim influence. Places such as Alexandria, Damascus, Tunis, Spain, the Byzantine lands, Persia, and India had been urban and intellectual centres for many centuries when the Arab armies arrived. So people who had long been trained in the ways of research, study, debate, and invention were eager to continue their work within the Arab context. Thanks to Arab and Muslim scholars, ancient Greek knowledge, acquired from their contact with Byzantine scholars, was kept alive and was eventually transferred to the West in the twelfth century and after. But not only did Arab and Muslim scholars preserve the heritage of Greek science and philosophy, they added to it by writing commentaries and glossaries, thus adding to what eventually became the Western intellectual tradition.
The Muslim civilisation covered a period of roughly nine centuries, from the middle of the seventh to the end of the fifteenth century, when the Muslim world was divided into three independent states, the Ottoman based in Turkey, the Safavid based in Persia, and the Mughal covered the Indo-Pakistan subcontinent. In the eighteenth and nineteenth centuries, Islamic regions fell under the sway of European imperial powers. Following World War I, the remnants of the Ottoman state became European protectorates [1–18].
The Development of Arab Medical Sciences
The health care practices of the medieval Muslim world over a large area and nine centuries were not uniform. The everyday practices and the public health were affected by many factors: fasting laws and dietary regulations during the holy month of Ramadan, hygiene and burying the dead by Muslims as well as by non-Muslims, the climatic conditions of the vast area, the living conditions of nomadic, rural, and urban communities, the amount of travel undertaken or commerce, or for pilgrimage, the maintenance of a slave class and slave trade, the injuries and diseases attendant upon army camps and battles, and the incidence of plague and endemic diseases [4–6].
As mentioned above, the Abbasids moved the Islamic capital to Baghdad by the tenth century. The city became the centre of scientific knowledge and research activity and emerged as the capital of the scientific and cultural world. In addition to Baghdad, Seville, Toledo, Granada, and other cities established themselves as centres for medical sciences. The eagerness of the rulers and society for learning resulted in the translation of substantial amounts of Greek, Persian, and Indian medical texts into Arabic. During the Golden Age, collaborative works of physicians and scientists from different nations and ethnic groups raised the dignity and calibre of the medical profession. Disease was seen by physicians as a problem that can be challenged. The Prophet (PBUH) was credited with many statements on health care problems and their treatments. For instance, “The one who sent down the disease sent down the remedy.” and “For every disease, God has given a cure.” He was also credited with articulating several specific medical treatments, including the use of honey, olive oil, figs, and cupping. But most importantly, whereas other societies usually feared the sick and afflicted, at best isolating them and at worst leaving them somewhere to die, the Prophet had a very compassionate and forgiving view of the sick.
As a result, health care services rose in esteem from that of a menial calling to the rank of a learned profession. It had advanced from ephemeral talisman and theology to real hospital wards, mandatory examination for doctors, and the use of technical terminology. Baghdad and Cairo had hospitals that were open to both male and female patients staffed by attendants of both sexes. These hospitals contained libraries, pharmacies, intern systems, externs, and nurses. There were mobile clinics to reach the disabled, the disadvantaged, and those in distant areas, regulations were imposed by the health authorities to maintain quality control on drugs, medical ethics was introduced, and pharmacy became separated from medicine and a licensed profession.
Baghdad and Cordoba became the main centres for development of herbal medicines. Al-Zahrawi (Albucasis, tenth century) of Cordoba wrote The Book of Simples, an important source for European herbal medicine. The Andalusian botanist Abu al-Abbas al-Nabati introduced the use of experimental scientific methods in the thirteenth century. He also introduced empirical techniques in the testing, description, and identification of numerous materia medica. Al-Nabati separated unverified reports from those supported by actual tests and observations. This allowed the study of materia medica to evolve into the science of pharmacy. Later on, Ibn al-Baitar, who lived in Damascus, published The Book on Drinks and Foods, a collection of different drinks and foods. It is considered as one of the most prestigious books in the medieval pharmacopeia in which the drugs are classified in alphabetical order. Other pharmacopoeia books include that written by Abu- Rayhan Biruni in the eleventh century and Ibn Zuhr (Avenzoar) in the twelfth century. Daoud al-Antaki used different herbs for treating patients and published a book on medicinal herbs summarizing the knowledge of his predecessors. Al-Antaki in the sixteenth century described in his book 57 plants that were used as a source for simple drugs, or frequently as one ingredient in complex herbal-based preparations. He described the plant and the way it was used by physicians. For instance, birthwort, carob, castor oil plant, common fennel, common myrtle, Persian cyclamen, saffron, serapias, sycamore fig, and Syrian bryony. Furthermore, Al-Antaki mentioned foreign plants that were brought to the area for their medicinal properties, such as cornelian cherry, purging croton, and gardenia. He also described pharmacological uses of typical agricultural crops, such as caraway, carrot, wild coriander, pear, quince, sugar cane, and walnut.
The development of medicine and pharmacy in the Muslim world laid the foundations for the development of modern Western medicine and pharmacy. Scholars from Muslim civilisation contributed many insights of their own to the development of medicine while acknowledging the knowledge they received from other civilisations. It is important to mention that they translated classical medical texts not only from Greek, but also from Persian, Indian, and Chinese sources. This synthesis resulted in a richer and universal medical system, based on scientific rules and experimentation. Al Tabbari (838–870), Al-Razi (Rhazes, 864–930), Al-Zahrawi (Albucasis, 936–1013), Al-Biruni (973–1050), Ibn Sina (Avicenna, 980–1037), Ibn al-Haitham (960–1040), Ibn al-Nafis (1213–1288), Ibn Khaldun (1332–1395) (Figure 3), Ibn al-Baitar (1197–1248), and Ibn Zuhr (Avenzoar, 1091–1161) are regarded as among the great medical authorities of the medieval world and as physicians whose textbooks were used in European universities up to the sixteenth century. They made accurate diagnoses of plague, diphtheria, diabetes, gout, cancer, leprosy, rabies, and epilepsy. Avicenna’s and Rhazes’s works on infectious diseases led to the introduction of quarantine as a means of limiting the spread of these diseases. Other physicians laid down the principles of clinical investigation, drug trials, and animal tests, and uncovered the secret of sight. They mastered operations for hernia and cataract, filled teeth with gold leaf, and prescribed spectacles for defective eyesight. And they passed on rules of health, diet, and hygiene that are still largely valid today. Physicians of different languages and religions cooperated in building a medical organization whose outlines are still visible in current medical practices.
The development and the recognition of the independent, academically-oriented status of pharmacy as a profession charged with the preparation of safe and effective drugs started in Baghdad during Al-Mamun’s caliphate (813–833). The main objectives of pharmacists were directed not only toward the translations and interpretations of accumulated data on natural product-based drugs, but increasingly toward the search for the potential of natural products as sources for new drugs, and they even started to elucidate physicochemical properties of these products. Drugs were classified according to their effects on the human body, for example, diuretics (promote urination and thus expel toxins), expectorants (remove mucous accumulation), topical antiseptic cleansers, stimulants (prescribed to increase blood flow and raise energy level), tonics (general strength building and disease prevention), analgesics and anesthetics, digestive aids, and oral health agents. Pharmacists, or saydalaneh in Arabic, managed to introduce a large number of new drugs to clinical use, including senna, camphor, sandalwood, musk, myrrh, cassia, tamarind, nutmeg, cloves, aconite, ambergris, and mercury. They also developed syrups, juleps, and pleasant solvents such as rose water and orange blossom water as means of administering drugs.
The first pharmacy shop was apparently in Baghdad, founded in 762, and medicines were manufactured and distributed commercially, and then dispensed by physicians and pharmacists in a variety of forms: ointments, pills, elixirs, confections, tinctures, suppositories, and inhalants. Saydalaneh were required to pass examinations and be licensed and were then monitored by the state [1–18].

Ibn Khaldun (1332–1406). The fame of Ibn Khaldun in modern scholarship is due to his writing of the Muqaddimah, or “Introduction.” In the Muqaddimah, he laid the foundations of a new science, “Ilm al-Umran,” or the science of human social organization.
The selection of potential natural products as sources for new drugs was based on traditional knowledge developed in the pre-Islamic era based on a long history of trial and error, and then by theoretical and practical knowledge introduced by Islam. These include natural products mentioned in the Holy Quran or in the Hadith of the Prophet (PBUH), notably honey, milk, dates, black seeds, olive leaf, and olive oil.
In addition, theoretical and practical knowledge developed in other medical systems, which became available to scholars after the translation of foreign scripts, played a central role in developing new medicines. The works of Galen, Hippocrates, and the Indian physicians Sushruta and Charaka were translated into Arabic. Physicians developed hundreds of new natural product-based remedies. They were not guided by a long history of trial and error, but mainly by scientific methods, which led to the development of evidence-based medication. Avicenna discussed in his book, on simple drugs (materia medica), the nature and quality of drugs and the way that compounding them influences their effectiveness. He stated “You can tell the potency of drugs in two ways, by analogy and by experiment. We say experimenting leads to knowledge of the potency of a medicine with certainty after taking into consideration certain conditions.” Physicians of Muslim civilisation considered all components of existence with equal importance, from breath and body to the soul and matter; both spiritual and physical health are treated equally. Hence, the body should be treated as a whole and not just as a series of organs and tissues. Physicians noted that there are individual differences in the severity of disease symptoms, and in the individual ability to cope with disease and healing. Hippocrates thus laid the foundations of the modern theory that thoughts, ideas, and feelings, which he proposed to originate in the brain, can influence health and the process of disease. Rhazes supported this concept by his recommendation:
“The physician, even though he has his doubts, must always make the patient believe that he will recover, for state of the body is linked to the state of the mind.” Later on, Avicenna who defined medicine as “the science from which we learn the states of the human body with respect to what is healthy and what is not; in order to preserve good health when it exists and restore it when it is lacking” supported the views of Rhazes. He stated that “We have to understand that the best and most effective remedy for the treatment of patients should be through the improvement of the power of the human body in order to increase its immune system, which is based on the beauty of the surroundings and letting him listen to the best music and allowing his best friends to be with him.”
It is now clear that the mind and the body interact, influence, and regulate each other. The perception of stress can lead to production of “stress hormones” as well as mediators of the immune system, for example, cytokines and free radicals. Stress hormones act in a feedback pathway to regulate their own production and the production of certain immune products. These immune products act on the brain to modify behaviour and the ability to perceive and to respond to stressful challenges by inducing lethargy, fever, and vomiting.
Based on the recommendations of Rhazes and Avicenna, patients were treated through a scheme starting with physiotherapy and diet, and if this failed, drugs were used. Rhazes’s treatment scheme started with diet therapy; he noted that “if the physician is able to treat with foodstuffs, not medication, then he has succeeded. If, however, he must use medications, then it should be simple remedies and not compound ones.” Drugs were divided into two groups, simple and compound drugs. Physicians were aware of the interaction between drugs; thus, they used simple drugs first. If these failed, compound drugs consisting of two or more compounds were used. If these conservative measures failed, surgery was undertaken.
The Greek and Roman humour theory of the human body or humoralism had a great influence on the development of the Greco-Arab medical system. Hippocrates was the first who applied this idea to medicine and it became strongly accepted in the medical canon through the influence of Galen. The humoral theory was adopted and further developed by physicians of Muslim civilisation and it became the most commonly held view of the human body among European physicians until the advent of modern medical research in the nineteenth century [1–8].
Commonly Used Herbal Medicines and Diets in The Arab And Islamic World
Medicinal plants and their products have been used traditionally across the world for the prevention and treatment of almost all known types of diseases. Clinical and basic scientific research confirmed the efficacy and action mechanism of several plants for treating several ailments, including liver disease, diabetes, skin diseases, and hypertension. As a result, about 25% of the currently prescribed drugs are of herbal origin. For instance, milk thistle (Silybum marianum) has been shown to have clinical applications in the treatment of liver diseases, including toxic hepatitis, fatty liver, cirrhosis, ischemic injury, radiation toxicity, and viral hepatitis, via its antioxidative, antilipid peroxidative, antifibrotic, and anti-inflammatory properties. Furthermore, milk thistle has shown immunomodulating and liver regenerating effects. Another example is Nigella sativa (black seed). The seeds of this plant are known to have many medicinal properties and are widely used in Greco-Arab and Islamic medicine. Therapeutic potential and toxicological properties of the seeds have been extensively studied. A Medline search using “Nigella sativa” or “black seed” reveals more than 800 citations, including antioxidant, anti-inflammatory, antimicrobial, hypotensive, antinociceptive, choleretic, uricosuric, antidiabetic, antihistaminic, immunomodulatory, anticancer, and antifertility effects [1–8].
Food plays an important role in Arab–Islamic medicine in maintaining a healthy body, soul, and spirit. Muslims are commanded to follow a set of dietary laws outlined in the Holy Quran where almost everything is permitted, except what God specifically prohibited. Later on, when the Muslim world covered all of Arabia, half of Byzantine Asia, all of Persia, Egypt, the Maghreb (North Africa), and Spain, Arabs and Muslims became exposed to foreign and multinational culinary heritages. Furthermore, great developments in scientific fields, the establishment of “modern” hospitals, and growing socioeconomic conditions of Islamic empire increased the awareness of the relationship between food and health. During this period, a type of Islamic food therapy developed that was a blend of Quranic teaching and Greek medicine.
The foods favoured by the Prophet were dates, honey, olive oil, and black seeds. Concerning olive oil, he said “Eat olive oil and massage it over your bodies since it is a holy tree.” Black seeds were regarded as a medicine that cures and prevents all types of diseases. The Prophet once stated:
“The black seed can heal every disease, except death.” Dates are mentioned in 20 places in the Quran. The Prophet is reported to have said: “if anyone of you is fasting, let him break his fast with dates. In case he does not have them, then with water. Verily water is a purifier.”
Safety and Efficacy of Herbal Medicines
The widespread use and popularity have also brought concerns and fears over quality, efficacy, and safety of the “natural” products available on the market as well as the professionalism of practitioners. It is well known that adulteration, inappropriate formulation, or lack of understanding of plant and drug interactions can lead to adverse reactions that are life threatening or lethal to patients. Safety assessment of herbal-based preparations has often been neglected since traditional and prolonged use is usually considered evidence of its safety. Another important factor is the belief that these medicines are prepared according to the principles of the Greco-Arab tradition that forms the basis for the current conventional product. However, a history of traditional usage is not always a reliable guarantee of safety since it is difficult for traditional practitioners to detect or monitor delayed effects (e.g., mutagenicity), rare adverse effects, and adverse effects arising from long-term use. Most reports concerning toxic effects of herbal medicines are associated with hepatotoxicity although reports of kidney, nervous system, blood, cardiovascular, dermatologic effects, mutagenicity, and carcinogenicity have also been published in the biomedical literature. A systematic safety review of herbal medicine and the contribution of scholars of Muslim civilisation to toxicology are given in chapter 11of the present authors’ book[1]. Standards for safety, quality control, use of modern cell biology and biochemistry, and in vitro as well as in vivo techniques for the evaluation of medicinal plants are also discussed in chapter 8.
There is little doubt that the use of the concept of Greco-Arab and Islamic herbal therapy has shown remarkable success in healing acute as well as chronic diseases. As mentioned above, Arab and Muslim physicians were the first to use scientific methods in the field of medicine and pharmacy, including the introduction of quantification, animal testing, and clinical trials. Hospitals in the Arab–Islamic world featured the first drug tests, drug purity regulations, and competency tests for physicians. In his Comprehensive Book of Medicine, Rhazes documented clinical cases of his own experience and provided very useful recordings of various diseases. He also introduced urinalysis and stool tests. Avicenna (980–1037) introduced experimental medicine and systematic experimentation and quantification in physiology. He discovered the contagious nature of diseases and described many medical treatments, including clinical trials, risk factor analysis, and the idea of a syndrome in the diagnosis of specific diseases. His book, The Canon of Medicine, was the first book dealing with evidence-based medicine, randomized controlled trials, and efficacy tests. Concerning the medical documentation, the first documented description of a peer-reviewed publication process was written by Ishaq bin Ali al-Rahwi (854–931). In his work, The Ethics of the Physician, he stated that a physician must always make duplicate notes of a patient’s condition. When the patient was cured or had died, the notes of the physician were examined by a local medical council of other physicians, who would review the practicing physician’s notes to decide whether the treatment had met the required standards of medical care.
Modern in Vitro and in Vivo Test Systems
Under international regulations, animal tests play a crucial role in developing new knowledge that provides the basis for a new drug development. The appropriate use of animals in biomedical research and safety testing is an indispensable part of the process for acquiring the knowledge necessary to control or treat disease and injury. Regulatory bodies worldwide require preclinical efficacy and safety data for new drugs based on animal tests before human clinical trials can be conducted. Animal studies are mandatory in order to reduce the risks for people and allow the safe creation of new therapies. Drug development is a time-consuming, costly, and complicated research process. Thousands of chemical compounds must be synthesized or purified (in the case of natural products) and tested in order to find a desirable therapeutic result. The Food and Drug Administration in the United States (FDA) estimates that it takes approximately 8.5 years to study and test a new drug before it can be approved for the general public. This estimate includes preclinical in vitro studies and animal testing, as well as clinical trials using human subjects. The appropriate and responsible use of animals is a mandatory part of biomedical research and pharmaceutical product safety testing. They significantly reduce the probability of side effects occurring during testing in humans. Around 70% of serious adverse effects that occur in humans are identified at the animal testing stage. In addition, animal tests enable researchers to determine which experimental compounds in advanced development are unsuitable for use in humans either because the risk of potential toxicity is too great or because they do not have the desired pharmacokinetic profile. Therefore, animal testing is extremely beneficial in minimizing the risks to humans in clinical trials. Culturing cells is the most widely used in vitro method in pharmacology, toxicology, and biomedical research. In general, in vitro test systems represent the first phase of the evaluation procedure.
Modern in Vitro And in Vivo Test Systems
In vitro cell culture methods have the advantage of relatively well-controlled variables and are generally accepted as a very effective method for safety testing. Advantages of these systems over classical methods, such as long-term studies on experimental animals, include relatively well-controlled variables, decreased costs, a reduced time to completion, and reduced number of animals necessary to complete the study. Although some advanced in vitro systems are available that allow prediction of the local effects of test pharmaceuticals, even the most sophisticated in vitro test cannot yet be used to measure systemic effects, for example, blood pressure or fever.
Given the well-known problem of using two-dimensional cell culture pharmaceutical test systems, more realistic three-dimensional tissue constructs are required in order to create more in vivo-like cell culture conditions, where cells and tissues do not exist in isolation but communicate with and are interdependent on neighboring tissue. The breakthrough might be to develop human three-dimensional in vitro test systems and tissue equivalents that could serve as in vitro model systems during the initial stages of drug discovery.
Drug Development from Herbal Sources and Regulatory Issues
Herbal-based drug discovery research is a multidisciplinary approach combining ethnopharmacology and traditional knowledge on the one hand and botanical, phytochemical, biological, toxicological, pharmacological, and molecular techniques on the other hand. As mentioned above, about 25% of the currently used prescription drugs contain at least one herbal-derived active ingredient and several herbal-based drugs either have recently been introduced to the market or are currently involved in late-phase clinical trials. Although herbal-derived compounds continue to provide an important source of new drug leads, numerous challenges are encountered including the procurement of plant materials, for example, the selection and implementation of appropriate high-throughput screening bioassays and the scale-up of active compounds.
It is generally believed that the standardization and regulation of plant materials is not required when used by the rural communities for their primary health care. Nevertheless, regardless of whether the medicinal plant is to be used by local communities or by industry, a systematic approach is required for a traditionally used plant, as is done in modern medicine. It is necessary to standardize all stages of herbal-based drug discovery: from cultivation, ethnopharmacology, utilization, isolation, and identification of active constituents to efficacy evaluation, pharmacology, safety, formulation, and clinical evaluation.
In general, many herbs are effective when consumed as whole or as extracts. Current trends, however, are directed toward the use of purified herbal-derived agents that can serve not only as new drugs themselves but also as drug leads suitable for optimization by medicinal and synthetic chemists. Even when new chemical structures are not found during drug discovery from medicinal plants, known compounds with new biological activity can provide important drug leads. In this respect, the sequencing of the human genome paves the ways for identification of thousands of new pathologically active molecules. With the help of modern in vitro and in vivo screening assays directed toward these targets, known herbal-derived compounds may show promising and possibly selective activity. Several known herbal-derived compounds have already been shown to act on newly validated molecular targets (e.g., indirubin selectively blocks cyclin-dependent kinases). Other herbal-derived compounds have also been shown to act on novel molecular targets, thus reviving interest in members of these frequently isolated plant compound classes [22-25].
References
- Esposito JL. The Oxford History of Islam. Oxford University Press, 2000.
- Hitti PK. History of the Arab. St. Martin’s Press, 1970.
- Saad B, Azaizeh H, Said O. Arab botanical medicines. In:Watson RR, Preedy VR (Eds.), The Encyclopedia of Botanicals in Clinical Practice. CABI Publishing, 2008.
- Saad B, Azaizeh H, Said O. Tradition and perspectives of Arab herbal medicine: a review. eCAM 2005;2:475–479.
- Pormann PE, Savage-Smith E. Medieval Islamic Medicine. Edinburgh University Press,2007.
- Morgan MH. Lost History: the Enduring Legacy of Muslim Scientists, Thinkers, and Artists. National Geographic Society, 2007.
- Bilal A, Jamal A. Unani system of medicine. Pharmacogn. Rev. 2007;1(2):210–214.
- Hajar Al Bin Ali HA. History of medicine. Heart Views December 2001–February 2002; 2(4).
- Deuraseh N. Health and medicine in the Islamic tradition based on the book of medicine (Kitab al-Tibb) of Sahih Al-Bukhari. JISHIM 2006;5:2–14.
- Said O, Zaid H, Saad B. Greco-Arab and Islamic herbal medicine and cancer treatment/ prevention. In: Watson RR, Preedy VR (Eds.), Bioactive Foods and Extracts: Cancer Treatment and Prevention, Taylor & Francis Group, 2009.
- Saad B, Azaizeh H, Abu Hijleh G, Said O. Safety of traditional Arab herbal medicine. eCAM 2006;3:433–439.
- Ibn Sena(Avicenna). Al Qanun Fi al Teb. Book 6. Dar Alfiker, Bairut, Lebanon, 1994, pp 77–78 (in Arabic).
- al-Antaki D. Tadhkirat Uli l-al-Bab wa l-Jami li-L-‘Ajab al-‘Ujab. Cairo, 1935 (in Arabic).
- Ibn Albitar. Aljamea Limufradat Aladwiya Walaghdiya. Dar Bulaaq, Cairo, 1974 (manuscript from twelfth century).
- Souayah N, Greenstein JI. Insights into neurologic localization by Rhazes, a medieval Islamic physician. Neurology 2005;65:125–128.
- Ar-Razi. Kitab al-Hawi Fi Al-Tibb li-Muhammad Ibn Zakariyya ar Ra-Razi, Vol. 1Al-Osmanya, Hyderabad, 1956.
- Ar-Razi.In: Al-Bakry Al-Siddiky H (Ed.), Al-Mansuri Fi Al-Tibb (The Book of Medicine for Mansur) Institute of Arab Manuscripts, Arab League Educational Cultural and Scientific Organization, Kuwait, 1987(in Arabic).
- Abun-Nasr J. A History of the Maghrib in the Islamic Period. Cambridge University Press, 1987.
- Pak E, Esrason KT, Wu VH. Hepatotoxicity of herbal remedies: an emerging dilemma.Prog. Transplant. 2004;14:91–96.
- Fugh-Berman A. Herb–drug interactions. Lancet 2000;355:134–138.
- Rousseaux CG, Schachter H. Regulatory issues concerning the safety, efficacy and quality of herbal remedies. Birth Defects Res. 2003;68:505–510.
- Imtara H, Kmail K, Touzani S, Khader M, Hamars H, Saad B, Lyoussi B (2019) Chemical analysis, cytotoxic and cytostatic effects of twelve honey samples collected from different regions in Morocco and Palestine, Evidence based complementary and alternative medicine Volume 2019, Article ID 8768210, 11 pages
- Shanak S, Saad B, & Zaid H (2019) Metabolic and Epigenetic Action Mechanisms of Antidiabetic Medicinal Plants. Evidence based complementary and alternative medicine Article ID 3583067, Volume 2019 (2019)
- Saad B, (2015) Integrating traditional Greco-Arab and Islamic herbal medicine in research and clinical practice. In Phytotherapies: safety, efficacy, and regulation, Ed. Igbal Ramazan. Wiley-Blackwell John Wiley & Sons, Inc.
- Saad B, (2019) Prevention and Treatment of Obesity-Related Cardiovascular Diseases by Diet and Medicinal Plants. In “Herbal Medicine: Back to the Future, Volume 2: Vascular Health. Edited by Prof. Ferid Murad, Prof. Atta-Ur-Rahman, and Prof. Ka Bian, Bentham, pp 125-165.
BASHAR SAAD, PhD, is Professor of cell biology and immunology at the Arab American University in Jenin, Palestine, and at Al-Qasemi Academic College, Baga Algharbiya, Israel. He made a significant contribution in combining cell biology, immunology, and 3D cell culture techniques with Arab-Islamic herbal wisdom. His research interests include antidiabetic, anti-inflammatory and anticancer properties of medicinal plants. He has written more than 150 original papers as well as review articles and book chapters on Arab-Islamic herbal medicine.
[1] Bashar Saad and Omar Said, “Greco-Arab and Islamic Herbal Medicine: Traditional System, Ethics, Safety, Efficacy, and Regulatory Issues”, 2011 John Wiley & Sons, Inc.










.png)











No hay comentarios:
Publicar un comentario